Biological Sensor Detects Hazards
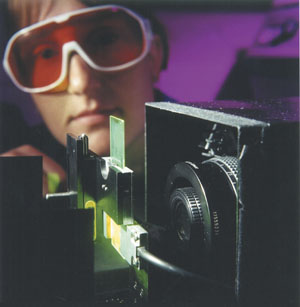 |
| Argonne National Laboratory scientist Susan Hammond tests a biochip in an Argonne-developed portable slide reader. Argonne researchers are developing a rapid, portable biological sensor that could provide greater protection for deployed troops as well as for first responders. |
Researchers are developing a portable sensor to detect hazardous biological materials more rapidly than current methods allow. The sensor has applications for government and private organizations and could be used to reduce the impact of biological weapons of mass destruction and to identify contaminants in health-related concerns.
The Argonne National Laboratory,
In the defense sector, the U.S. Army has taken the current Biochips model to detect substances such as anthrax. “Most of the more dangerous things are being handled by equipment we’ve handed off to the Army,” says Patrick Wilkey, director of the Center for Environmental and Security Science and Technology at
Biochips is an analytical laboratory that comprises reusable slides, also known as biochips, and a portable reader. Hundreds of thousands of gel pads, or gel dots, are placed on each slide. The gel pads contain segments of known nucleic acids, proteins, peptides and other similar biological substances that tailor the gel pads to recognize a specific biological agent or biochemical signature. When an unknown material or suspected biohazard comes in contact with the gel pads, the substances in the pads hybridize with the source material, identifying the unknown agent.
Different gel pads on the slide can have various biological substances, allowing each slide to identify more than one specific biological hazard at a time. For instance, a cluster of 100 gel pads could store specific DNA, and another 100 gel pads could contain different DNA. The test conductors know the locations of the various gel pads.
To begin the experiment process, the unknown source material is tagged with a fluorescent before being pushed across the field of gel pads. The user then lets the gel pads and unknowns hybridize, building linkage in the materials. When the slide is put into the portable reader, which illuminates the biochip from the side, any positive matches result in a fluorescent glow. “You end up getting a pattern,” Wilkey says. “Using that pattern, you can identify the individual material you’re looking at.”
As the technology currently stands, users must have a general idea of what substance they are looking for in order for the biochips to work effectively.
The biological materials in the gel pads and the substances they eventually will detect are being developed concurrently. This parallel development is a key component to Biochips, Wilkey notes, so scientists can ensure that they get a proper match.
Scientists are pursuing research in veterinary and human biology fields to develop the Biochips product. Wilkey expects that as researchers look more at veterinary diagnostics, they will find more of the materials they need for use in the gel pads.
 |
| Anne Gemmell, an Argonne scientist, places biological material on a slide. When biological hazards come in contact with the slide, also known as a biochip, the substances on the biochip link with matching biological hazards, allowing users to identify contaminants. |
Researchers also are working on eliminating false negatives and false positives. Wilkey explains that the samples Biochips users would and do work with are dirty samples—impure substances are mixed with the material users try to identify. A dirty sample creates a weaker match than a purer sample and also can lead to false results. The Biochips development team found a way to heat the slide to melt off the weak matches and leave only the strong matches, resulting in a more accurate reading.
Wilkey believes further developments and improvements to Biochips will play a critical role for
In addition to determining whether an area is safe, troops who encounter a substance that makes them ill can use the Biochips technology to help identify the cause of the illness quickly, preventing a ripple effect to other troops and enabling affected soldiers to receive the right care sooner.
Project developers are finding ways to make the technology smaller and more portable. In its current form, Biochips is not a field-portable instrument; however, the development team envisions service personnel using this version in mobile laboratories in forward positions.
The only requirements for operating the system are a power source, a clean laboratory space and a qualified technician. In the future, developers plan to provide a disposable cartridge with all sample preparation included, allowing a field medic to place a fluid sample on a card, insert it into the battery-powered imager and wait for an output. The imager also may be able to send data back to field hospitals. Field use of Biochips, both in its current and future forms, allows the identification of biological hazards before infected troops are moved to densely populated hospitals.
Despite the current emphasis on biological weapons, Wilkey says his team has worked steadily on the biological sensor’s development for the past 10 years with no big surges in workload recently. As for human health threats such as avian flu, which Wilkey calls the “threat du jour,” the technology could be used in their detection as well and they do not change the work of his team, he says.
Influences that do affect the team’s focus include new sponsors and their objectives. Funding comes from diverse sources such as the U.S. Defense Department, the National Institutes of Health, the U.S. Department of Homeland Security and the private sector. Wilkey says
Web Resources
National Institutes of Health: www.nih.gov




Comments