Lasers Shine a Light on Human Tissue Regeneration
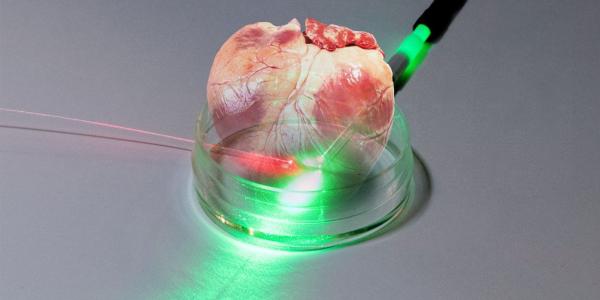
A new, highly precise photon sensor could help advance the science of growing human tissue, such as bones, skin or vital organs, in the laboratory and could benefit warfighters and society. The potential applications include monitoring environmental conditions, such as poison gases on the battlefield or toxins in the home.
Researchers at the National Institute for Standards and Technology (NIST) recently announced the development of a proof-of-concept sensor that measures temperature changes resulting from variations in pH levels, or acidity. Measurements of pH are a vital part of tissue engineering studies because as cells grow, their environment naturally becomes more acidic. If the environment becomes too acidic the cells die off.
Unlike conventional sensors, the low-cost thermometer could monitor the environment in a cell culture for weeks at a time without having to be recalibrated. It might also be used inside the body to monitor the immune system’s reaction to implanted organs. Further in the future, warfighters could volunteer to have their stem cells stored so that their own tissue, or entire organs, could be grown in the lab to help them recover from battlefield injuries.
The device uses commercially available, flexible optical fibers about the width of a human hair etched with a grating, or a series of lines. The grating acts as a filter for light that reflects certain wavelengths, or colors, while allowing others to pass. Changes in temperature or pressure alter the wavelengths of light that can pass through the grating. To adapt their photonic device for measuring acidity, the team added a coating for measuring minute changes in temperature resulting from changing levels of acidity.
Commercial pH instruments are highly accurate but require frequent calibrations to ensure accurate readings day to day. What’s needed for this kind of research is a measurement system that can stay for weeks at a time inside an incubator with the cells without needing to be removed or calibrated,” says NIST chemist Zeeshan Ahmed in the written announcement. “We want to make sensors that can be put inside growing tissue to give researchers quantitative information. Is the tissue actually growing? Is it healthy? If you grow a bone, does it have the right mechanical properties, or is it too weak to support a body?”
Matthew Hartings, an associate professor of chemistry at American University and a guest researcher with the NIST, illustrates the need with a personal anecdote. A relative, he reports, recently had a double lung transplant after waiting a long time for a donor. “If you get a liver transplant, someone had to die in order for you to get that liver. So, instead of harvesting those organs from someone who has recently passed, there’s a big push to grow those organs—or the start to those organs—in a lab,” he says. “You need to see that everything is growing the way it’s supposed to in the lab or in your body.”
The device, he elaborates, could be implanted in the body along with a new organ or growing tissue. “The sensor is great at measuring temperature so you can put this tiny width-of-a-hair thing into a tissue implant and measure the temperature.”
In the NIST announcement, Hartings compares the device to a navigational system. “What these sensors could give people is real-time information about tissue growth and disease progression.”
New hips, knees or other implants result in cells communicating through chemical changes. “The cells communicate to one another by throwing out little chemical breadcrumbs. One of the things we’re trying to do is to come up with a way to track some of these bread crumbs in real time without having to go do lab work,” Hartings says. He adds that after her surgery, his relative “was having blood tests every day, and then it went to every week and then every month and then every little bit.”
The researcher suggests that advances in body tissue regeneration could one day benefit warfighters on the battlefield. “If one of our warfighters has a leg shredded from an [improvised explosive device] and they don’t have to lose a leg but the bone is just a mess of broken pieces, there are folks who are working on bone replacement scaffolds that you can insert into our soldiers and have them heal and grow bone naturally in that environment,” he offers. “There are scientists who are working on replacing shattered bones in arms or legs.”
Another team of researchers recently announced a 4D-printed scaffold that can be shaped into complex designs with multiple curves similar to a human face. That research might one day become a scaffold inserted into the body to help grow muscle, skin or bone. (See page 16)
The Defense Department could ultimately create a bank of stem cells for military members. “For any warfighter who goes into battle or enlists in the armed services, we could have a bank of their stem cells extracted from their bodies just on the chance that they are hurt in battle and we need to start growing a new bone for them, or a new liver or whatever the case may be,” Hartings theorizes.
The new sensor could have other uses as well, including detecting dangerous toxins on the battlefield. Hartings notes that some researchers are developing materials that can be used in gas masks to break down toxins and render them harmless. Those materials could be added to the photonic sensor in place of the current pH-sensing coatings. “Invariably, in that process of breaking those toxic chemicals down, you will get a heat release or a change in temperature. I can easily see coating one of our thermometers with one of these materials,” he says, explaining that the resulting temperature change would be an early warning sign that “mustard gas or sarin is in the environment” and warfighters “need to mask up right now.”
The technology also might have an array of commercial uses. Hartings indicates, as one example, that new carpet or new cabinets can result in higher levels of formaldehyde in a home. “I think there’s a big chance to study indoor environmental toxins. It’s a research area that’s really starting to pick up steam. People are interested in studying how chemicals in our indoor environment affect our health and how we go about measuring those.”
Additionally, measuring pH levels is often a vital part of developing new medical treatments. “When a pharmaceutical company is making a new antibody or making a flu vaccine, pH is one of those processes they have to measure all the time,” Hartings points out.
Currently, those companies use relatively bulky pH-measuring electrodes that can cost $500 each and “go bad after a week of use.” The NIST-funded sensor, on the other hand, can be used continuously and might ultimately cost as little as $10. “You can imagine any number of other coatings that are meant to measure other chemical processes and other chemicals in the environment. Now, if you have a sensor that costs $10 instead of $500, it doesn’t matter if you have to throw it away after a week, but we also think we can use them for longer periods of time,” Hartings says, reporting that the sensor recently performed for a full month.
The chemist predicts that such bioindustrial uses will be the first application of the technology. “I think the quickest commercial use would be in industrial reactors. NIST being what it is—their charter and their mission statement is to help American business—and there is a real need within the bioindustrial community to measure pH.”
And it likely won’t be long before the team has a prototype. “We’re really working out the kinks. It’s going to be about a year and a half to two years before we can even start to think about marketing and selling it. That being said, we are very close to having prototypes that we can test. Having a prototype and having an industrial partner, that’s going to happen probably within the next year,” Hartings predicts.




Comment
Appreciate you for this
Appreciate you for this opportunity to illustrate various applications using laser optics and modern bio engineerings
Comments